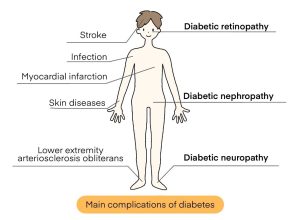
When blood sugar levels remain high due to diabetes, the following processes lead to retinopathy
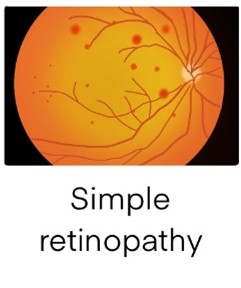
1. Simple retinopathy
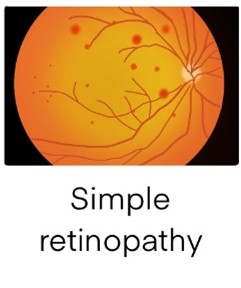
Simple retinopathy is the earliest stage of diabetic retinopathy. First, the capillaries in the retina begin to become fragile because of persistent high blood sugar levels. Eventually, blood leaks from the capillaries and proteins and lipids in the blood begin to deposit on the retina.
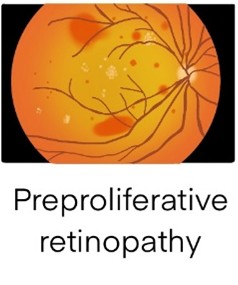
2. Preproliferative retinopathy
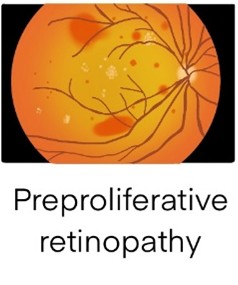
When simple retinopathy progresses to preproliferative retinopathy, the capillaries become clogged, and oxygen and nutrients cannot reach the inside of the retina. This condition is called preproliferative retinopathy, and the capillaries begin to show irregular shapes such as expanding and tortuous. Even at the preproliferative retinopathy stage, there are no subjective symptoms unless there is an abnormality in the macula in the center of the retina.
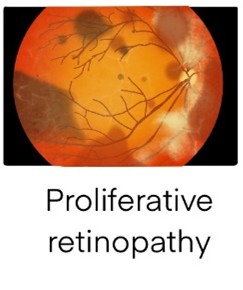
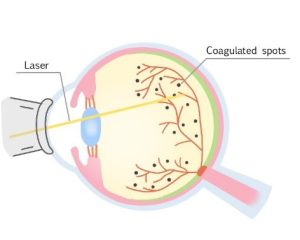
3. Proliferative Retinopathy
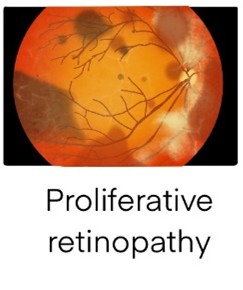
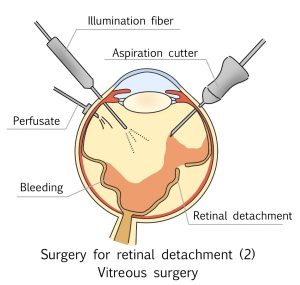
In the proliferative retinopathy stage, capillaries become blocked over a wide area, causing the retina to become oxygen-deficient. To compensate for this lack of oxygen, new blood vessels are formed in the retina.
However, the new blood vessels are fragile and prone to bleeding in the vitreous. Eventually, a tissue called a proliferative membrane forms around the new blood vessels. This can pull on the retina and cause retinal detachment. This can lead to vitreous bleeding, retinal detachment, and even glaucoma, which can lead to vision loss or blindness.
Symptoms of Diabetic Retinopathy
The mild stages of diabetic retinopathy, simple retinopathy and preproliferative retinopathy do not cause any symptoms and are often only detected during regular eye examinations.
If left untreated until vision loss begins and becomes noticeable, it becomes difficult to stop the progression and the risk of blindness increases.
Therefore, regular eye examinations are important for early detection.