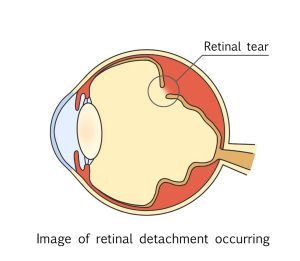
A typical retinal detachment begins with a retinal tear. If left untreated, the tiny hole allows vitreous fluid to penetrate between the retina and the layers underneath, eventually causing a retinal detachment.
Rhegmatogenous retinal detachment caused by a hole is most common in 20s and over 50s and older. People with severe myopia or a family history of retinal detachment are more likely to develop retinal detachment.
Age-Related Posterior Vitreous Detachment
The vitreous body inside the eye liquefies with age. When the liquefied vitreous separates from the retina, it can pull the retina apart, causing a hole or detachment of the vitreous and retina together.
Approximately half of people in their 60s and more than 70% of people in their 70s develop vitreous detachment, but in the case of myopia, it is said to occur about 10 years earlier.
Tear due to bruising or trauma
Some people may think of boxing when they hear the term “retinal detachment.” This is because a certain number of boxers suffer from retinal detachment due to the impact of receiving a punch. The impact of being hit by a baseball or soccer ball can also damage the retina.
High myopia
Myopia is often caused by an elongated eyeball. The longer the eyeball, the thinner the retina becomes, making it more susceptible to retinal detachment.
Atopic dermatitis and other diseases
Retinal detachment is also likely to occur in people with severe skin inflammation around the eyes, such as atopic dermatitis. It is thought that repeated rubbing of the eyelids due to itching puts pressure or impact on the retina, causing retinal detachment.
Other conditions, such as diabetes, may also cause this condition.