If symptoms of night blindness are present, the ophthalmologist will perform the following tests
Fundus examination
This is an examination to check the condition of the blood vessels in the fundus, the retina, and the optic nerve. In the case of retinitis pigmentosa, pigmentation and uneven deposition can be seen in the retina, but in the early stages or in mild cases, it may not be possible to confirm this, so observation is necessary.
Visual field test
This is a test to determine the extent of the visual field, or how wide the patient can see. Since retinitis pigmentosa and acquired night blindness tend to cause narrowing of the visual field, the test can be used to determine the stage of the disease.
Electroretinogram (ERG: electroretinogram)
This is a test to determine whether the retina is working properly. It examines the function of the retina by observing the electrical changes that occur when the retina is exposed to strong light.
If the function of rod cells, which function in the dark, is impaired, evoked potential becomes smaller or no response is observed.
Dark adaptation test
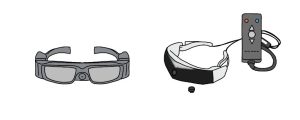
The dark adaptation test is used to determine the degree of night blindness. This test measures how the eye adapts to light when a subject moved from a brightly lit place to a dark room.
A dark adaptometer can be used to construct a dark adaptation curve and check the response of both cones and rods, the absence of rod response being characteristic of night blindness.
Optical coherence tomography (OCT)
OCT is a test that examines a cross section of the retina. If retinitis pigmentosa is advanced, this test can show areas of photoreceptor cell loss.
Fundus autofluorescence (FAF: fundus autofluorescence)
Autofluorescence is the emission of longer wavelength fluorescence after exposure to light of a specific frequency. The image is bright when there is a large amount of lipofuscin, a pigment present in the retinal pigment epithelium, and dark when the lipofuscin decreases as the disease progresses and the retinal pigment epithelium is damaged.
Regular check-ups are recommended to monitor the progression of the disease.
Other tests that may be performed if acquired night blindness is suspected include blood vitamin A levels, the presence of tumors, and the presence of autoantibodies against the retina.